“The baby is in cardiac arrest.”
Those words stun the parents of a 3-month-old, who arrived at the hospital with their sick child and now await word on their infant’s fate.
The team entrusted with that little life understands the responsibility to deliver immediate, and correct, care for the tiny patient.
That nerve-wracking scenario played out recently at the Dyersburg Regional Medical Center, but thanks to specialized training in pediatric emergency situations, treatment went smoothly and the child’s life was saved.
The Medical Education & Research Institute (MERI) provided the training that paramedics and hospital staff called on to save the child.The Memphis-based training school and bioskills lab creates and conducts hands-on educational courses to help healthcare providers improve their skills.

Recently it has turned its attention to pediatric hospital care in rural areas, particularly emergency situations, to meet a growing need, says Kaye Stewart, RN, MSN, simulation education coordinator.
The problem doesn’t lie in medical competency, Stewart is quick to point out. Rather, most emergency-room personnel, from physicians and nurses to the EMTs who provide initial care and transport, are far more used to working with adults.
This is especially true in rural areas, where care providers seldom see smaller children and so are less familiar with their special needs.
“Hospital emergency rooms aren’t set up for pediatric care,” Stewart says.
“Though 80 percent of pediatric cases are seen in adult facilities, they are a small fraction of the total patients. We knew we needed to help these people, who want to do the best job of taking care of those children.”
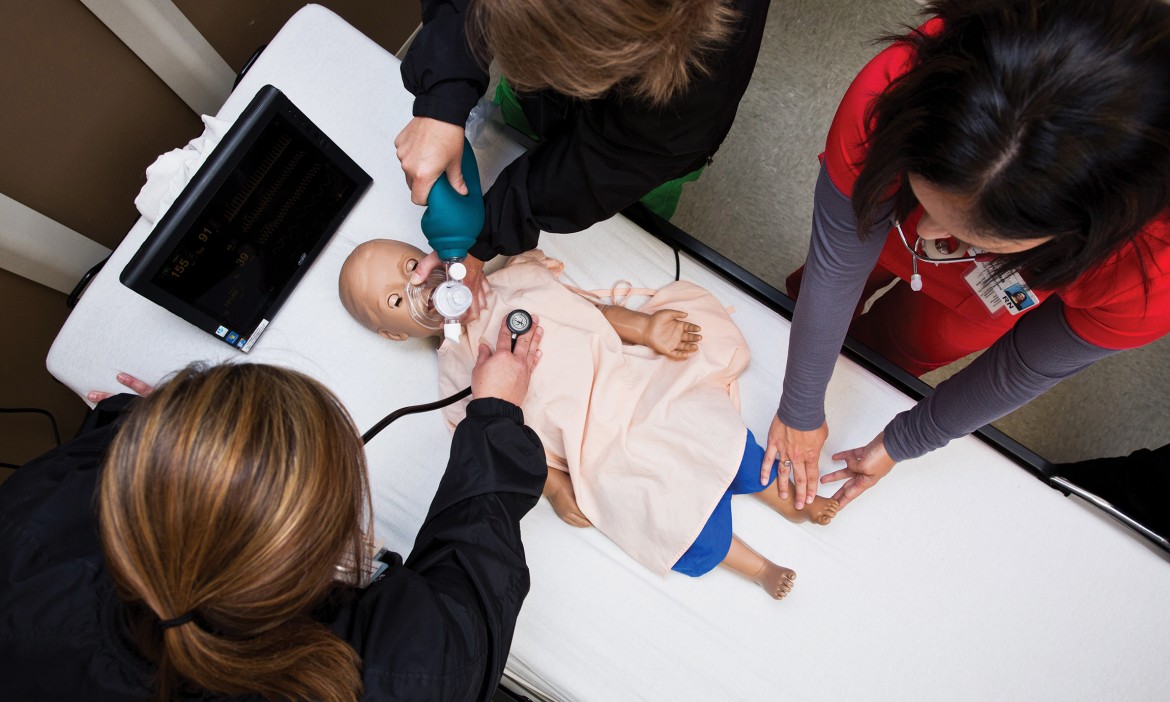
Hands-on training with an almost human patient
MERI’s corps of pediatric and adult mannequins — including a pregnant one called “Noelle” — get beyond classroom lectures to provide hands-on experience.
The mannequins simulate seizures, shock, respiratory problems ranging from mild difficulty to bronchitis or asthma, and even cardiac arrest.They respond to a computerized program, so the nurses, doctors and other trainees never know what’s going to happen.
One course of treatment may not work, meaning they have to shift gears and problem-solve in a realistic, timed situation. It’s both more challenging and helpful than working out theories on a chalkboard or tablet.


“Being able to get those human-patient simulators was wonderful for us,” says Janie Bard, RN, CPN, director of the medical-pediatric and medical-surgical units at Dyersburg Regional Medical Center.
“We put all the nurses in our OB department through training for delivering a baby with complications. That made the learning experience 110 percent better than just sitting and talking about it. You respond, take an action, and then see what results that action has.”
The enhanced training folds in as many people as possible, from paramedics and transport teams to clinicians throughout the hospital. This focus on pediatric issues can make a world of difference at rural facilities, as they seldom have pediatric specialists on staff.
“They are smaller, more remote and have tight budgets,” says Diana Kelly, manager of institutional development for MERI.
“We work with Le Bonheur Children’s Hospital for these trainings, because they know the patients from these rural areas, and that lets us create meaningful, real-life situations for the simulations.”
Training to triage
Bard was on hand at the hospital recently to see just how meaningful the training is.
“We were in the nursery working with the newborn mannequin when a 3-month-old was brought in with respiratory arrest,” she recalls.
“We’d just been participating in that simulation, and now had to perform that care on a real baby.”
Not every simulation will lead to such quick real-time application, but the enhanced skills will, over time, lead to more children being able to stay in their community for care, or if relocation is necessary, it will be more efficient.

“The quicker we identify what’s going on with a child, the quicker we can get on the phone to the receiving facility, and prepare everything needed for the transport,” Bard explains.
“Then we’re doing a better job for that patient, and the receiving hospital is more prepared for what’s headed their way.”
Ultimately, the MERI-led training is giving caregivers the skills they need to do what they do best: care.
“This partnership has allowed everyone here to work with pediatric patients 10 times better,” Bard says.
“It’s a great partnership. We’re not just teachers and students, but all part of a team.”
“We use our own departments, our own equipment, so everyone is comfortable and we know we have everything we need in a real-life situation. Everyone is more confident, and that really calms down the patients and their parents.”
“The last thing you want to see is somebody fumbling around when it’s your kid,” agrees Stewart.
“We are able to train people who then can go on and train others within the facility. A lot of medical providers are scared to work with kids, because they have children of their own and it’s very personal.
“They are very eager to get any kind of education which makes them more comfortable, and this program has really provided that to them.”